30 Oct Back to the future
Huge advances in technology are helping spinal surgeons achieve better outcomes for patients in ways that were never previously possible.
There have been vast improvements in spinal surgery over the past 30 years. Most have been facilitated by technology that allows surgeons to better visualise spinal anatomy and pathology.
Before CT, MRI and other imaging techniques became available, spinal surgeons relied on clinical examination alone to pinpoint the problem area – essentially sophisticated guesswork.
Today’s neuro-imaging allows a surgeon much more precision in diagnosis and treatment.
Improved technology means surgeons can plan each surgery more accurately and perform operations with the smallest possible incisions and tissue disruption – a concept called ‘‘minimally invasive surgery’’. Less tissue disruption can lead to swifter patient recovery times.
Most spinal surgery is performed to decompress nerves within the spine. However, in some cases, spinal instrumentation such as disc replacement surgery and fusion surgery is required to achieve the best outcome.
‘‘This type of spinal surgery has attracted a negative press in recent times but, done well and for the correct indications, it can be an extraordinarily effective remedy with outcomes equivalent to hip replacement surgery,’’ says Dr Yanni Sergides, a Sydney spinal neurosurgeon.
‘‘The first major advance in spinal instrumentation was the pedicle screw,’’ Dr Sergides says. ‘‘This allowed doctors to perform spinal fusion far more effectively and to mobilise patients immediately after their surgery.
‘‘The screws are designed to stabilise the vertebral column and allow the surgeon to fix weak or degenerating areas of the spine.’’
Surgeons have an extensive arsenal of implants and instrumentation at their disposal. There are more than 30 discreplacement devices available, as well as devices that are designed to stabilise the spinal column without fusing it – motion preservation prcedures.
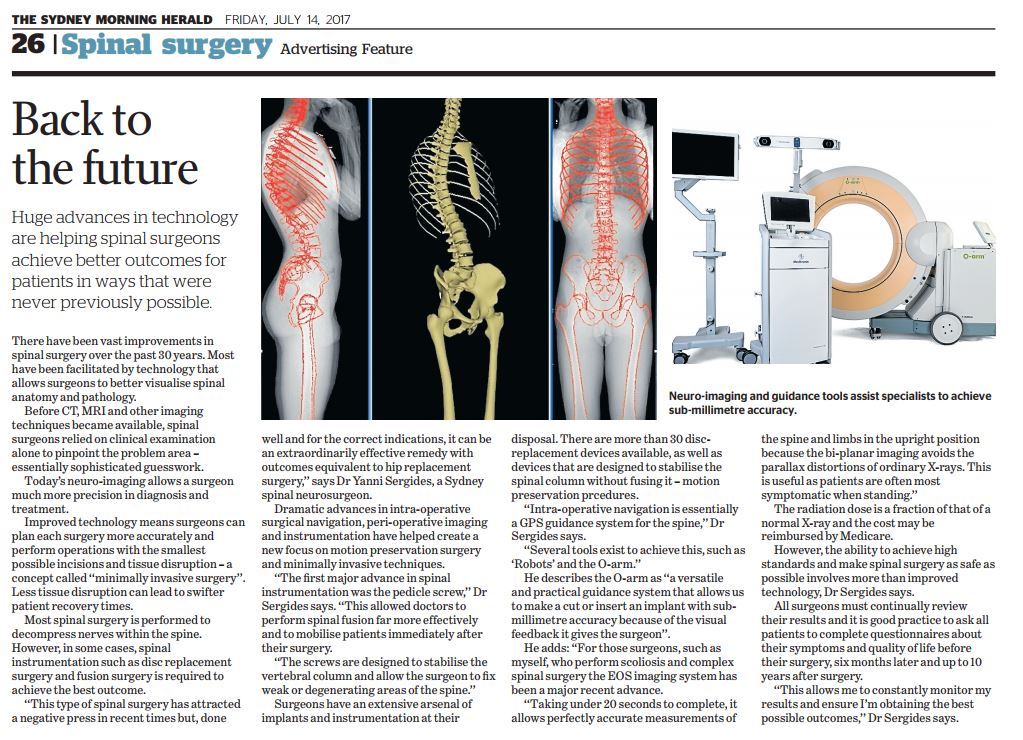
‘‘Intra-operative navigation is essentially a GPS guidance system for the spine,’’ Dr Sergides says.
‘‘Several tools exist to achieve this, such as ‘Robots’ and the O-arm.’’
He describes the O-arm as ‘‘a versatile and practical guidance system that allows us to make a cut or insert an implant with submillimetre accuracy because of the visual feedback it gives the surgeon’’.
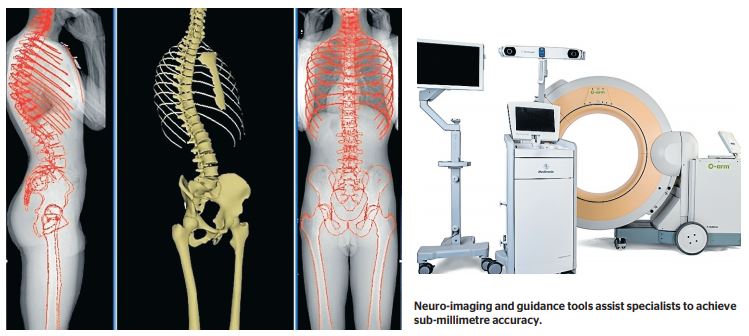
He adds: ‘‘For those surgeons, such as myself, who perform scoliosis and complex spinal surgery the EOS imaging system has been a major recent advance.
‘‘Taking under 20 seconds to complete, it allows perfectly accurate measurements of the spine and limbs in the upright position because the bi-planar imaging avoids the parallax distortions of ordinary X-rays. This is useful as patients are often most symptomatic when standing.’’
The radiation dose is a fraction of that of a normal X-ray and the cost may be reimbursed by Medicare.
However, the ability to achieve high standards and make spinal surgery as safe as possible involves more than improved technology, Dr Sergides says.
All surgeons must continually review their results and it is good practice to ask all patients to complete questionnaires about their symptoms and quality of life before their surgery, six months later and up to 10 years after surgery.
‘‘This allows me to constantly monitor my results and ensure I’m obtaining the best possible outcomes,’’ Dr Sergides says.

